Boost Retention and Acquisition
Leverage member-specific decision factor analysis to boost Age-In, Prospect Acquisition, and Retention rates. Enjoy proven 15% improvement above baseline and an additional 5% year over year.
Who Will Enroll in
Which Plan and Why
Through claims and demographic data analysis, we help health plans understand the key considerations and motivation of members to enroll or remain in a plan.
HBM analysis outputs help plans highlight the need to switch or retain a plan way before the annual AEP starts. This is achieved through personally relevant communications based on individual member concerns and motivators, delivering more effective results faster.
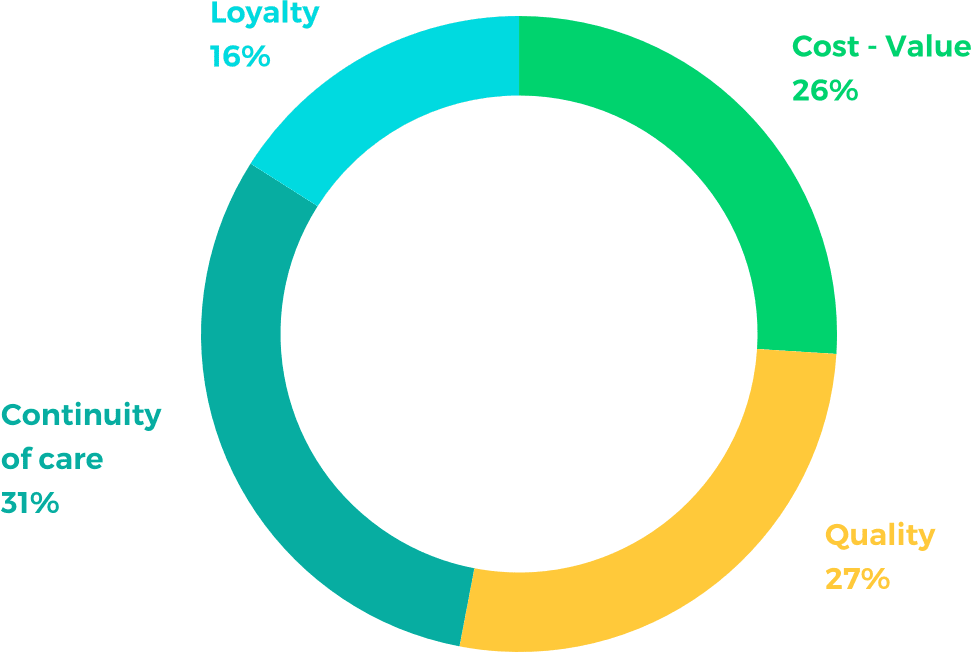
Why Do Members Stay?
In reality, members’ health decision factors stem from varied phenotypes and underlying motives. If, for example, a member has a “Continuity of Care” concern, HBM technology weighs the importance of that decision factor and the motivation behind it in order to create effective personally relevant communication.
with Medorion HBM generated member experience
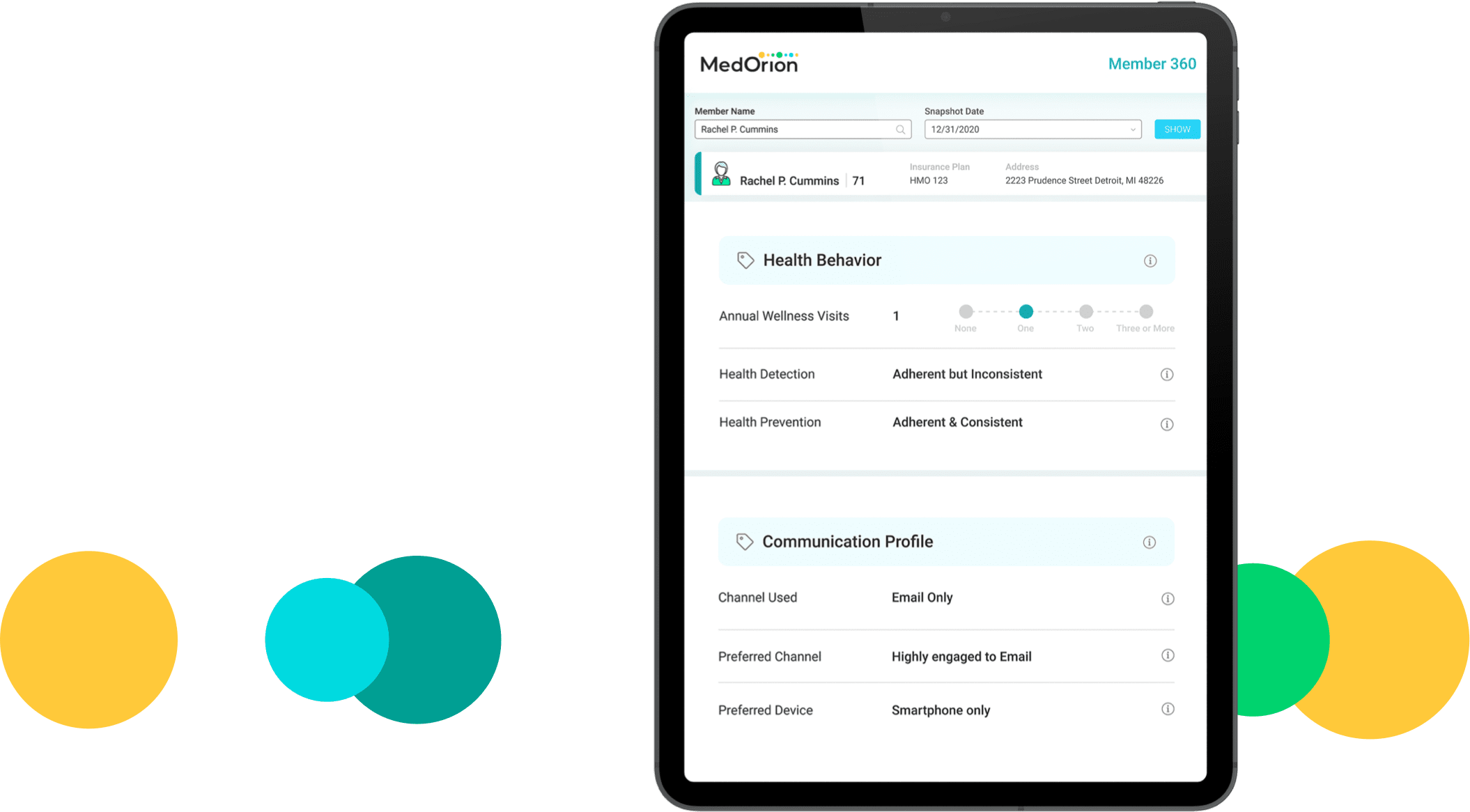
Build Lasting Relationships
Ongoing individual level insights and automatic health behavior transformation iterative learning through HBM AI, provides health plans with a unique benefit: Navigating member experience in real time to considerably improve the member-plan relationship in the long run.
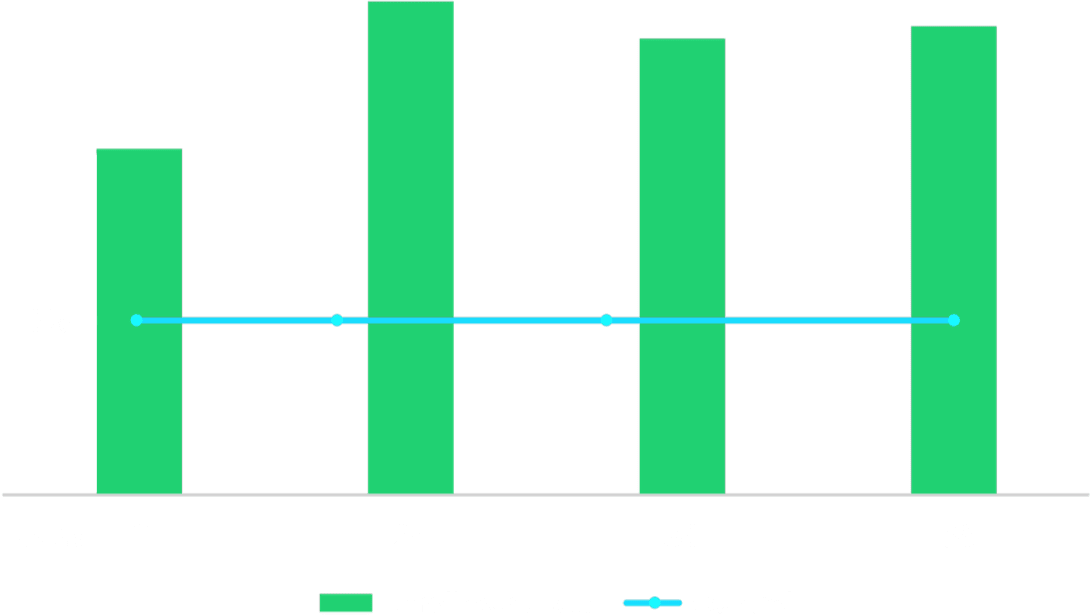
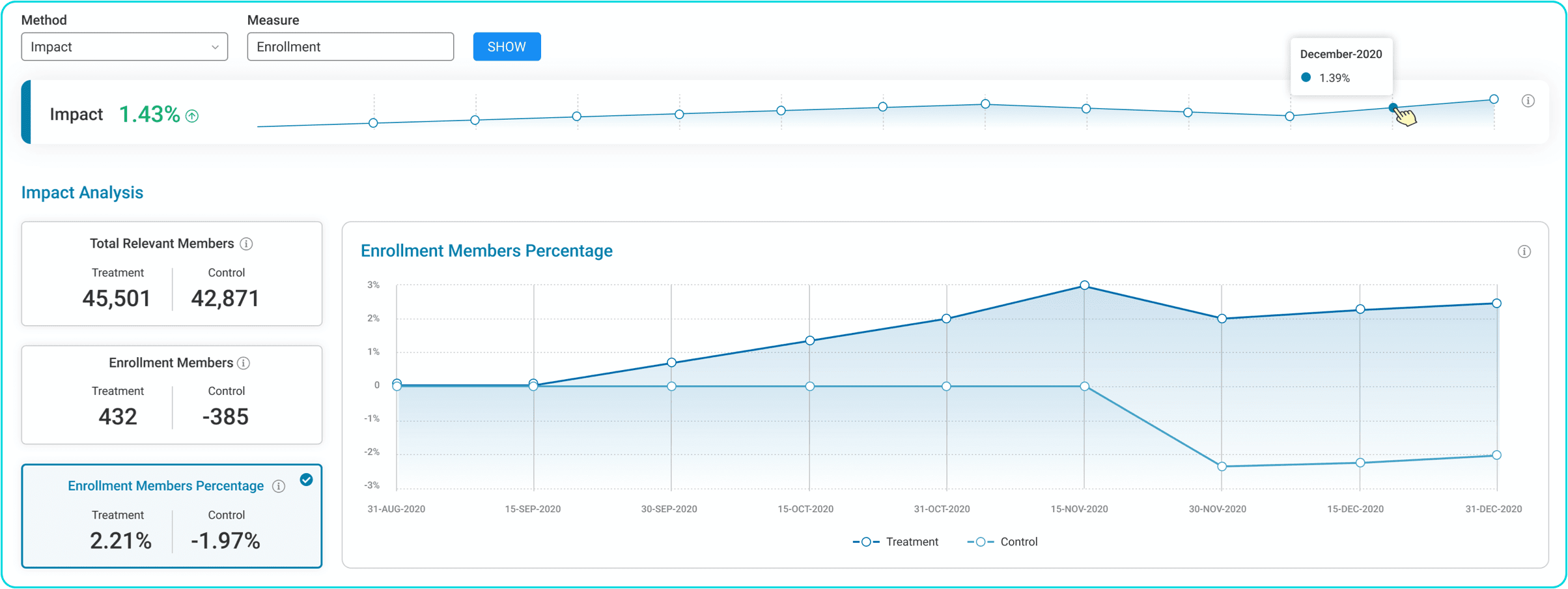
Real Time Impact Monitoring
An interactive dashboard displays HBM’s impact on enrollment rates in real time. AI-based continuous learning enables monitoring, reporting, and analytics of member experience. This yields a deeper understanding of members’ reasons not to enroll, their likelihood to enroll, and how they can be driven to do so.
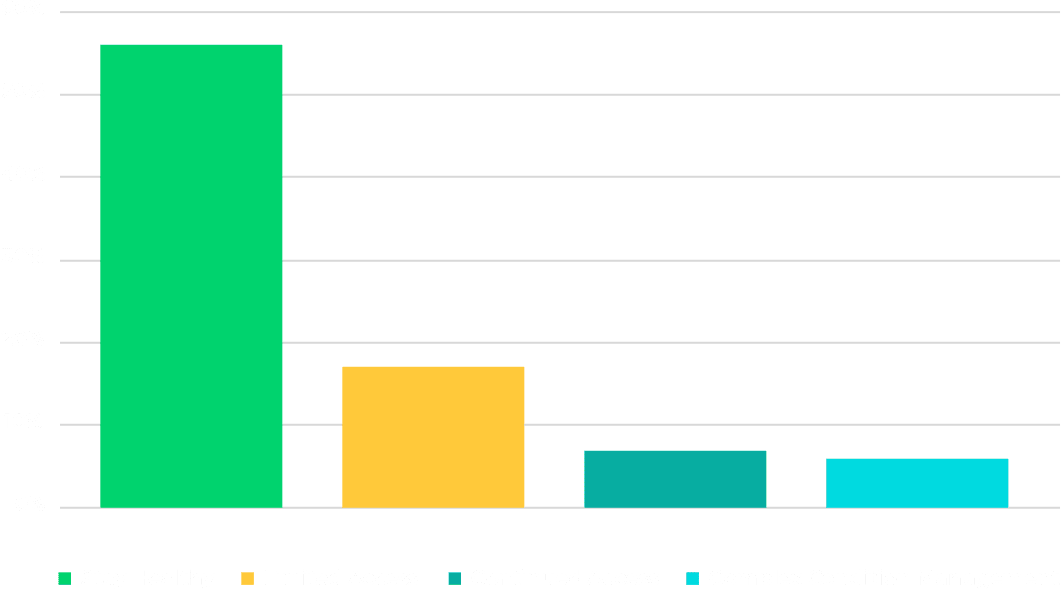
Medicare Advantage Age-In Prospects, Acquisition, And Retention
The HBM Always On Medicare Advantage Marketing
solution deployed within a large US-based health plan,
showed higher enrollment results vs. a control group. This improvement rose over time.