

Improve Quality Measures with Electronic Behavioral Record (EBR) Technology
MedOrion’s SaaS solution empowers leading health plans to improve member adherence by leveraging behavioral science and AI.
Our platform identifies individual barriers to care, persuades members to engage, and closes gaps at scale, driving better health outcomes
Our Solutions
We help health plans achieve better member health and improved financial outcomes.
For all members. Impacting all measure outcomes. Across all lines of business.
Retention & Acquisition
Boost Age-In and Prospect acquisition, improve retention rates for Medicare Advantage, Medicaid, and Individual Plans.
Clinical Quality
Increase Medicare Advantage star ratings by ½ - 1 star by increasing member adherence to HEDIS measures.
Pharmacy
Gain 1-2 stars for each of 6 HEDIS and Part D Pharmacy Measures within 12 months.
Member Experience
Improve member responses to CAHPS and HOS surveys by driving valuable member actions.
Trusted by Top National and Blue Health Plans




Real Time Health Behavior Transformation
Adapt to real-world settings by understanding individuals’ barriers in real-time.
Own and govern member experience.
Scale up accurately to improve the health and financial outcomes of the entire member base.
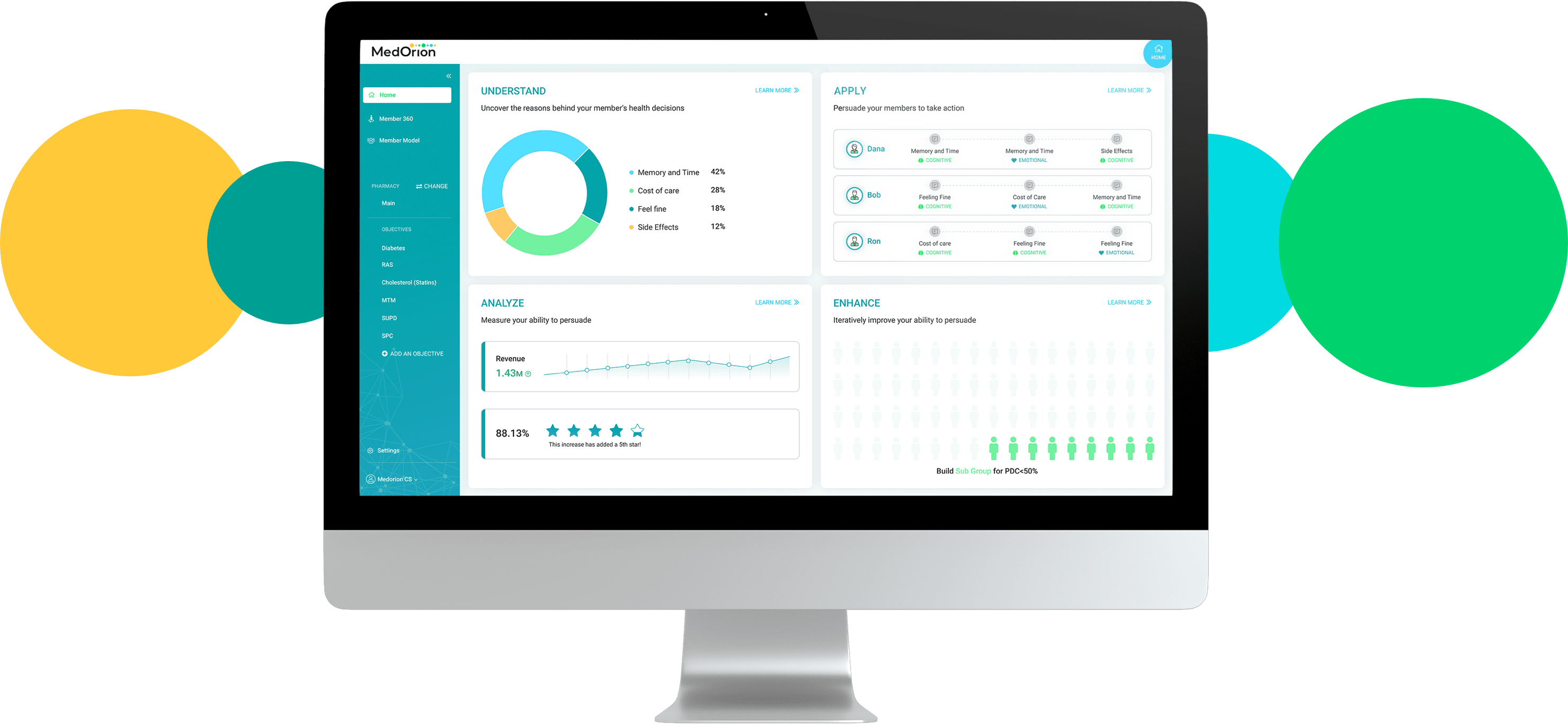
MedOrion’s EBR at Work
Let's Connect
Have a question about how EBR technology can help your organization? We’d love to hear from you.


