Automatically Leverage Member-level Decision Barrier Analysis
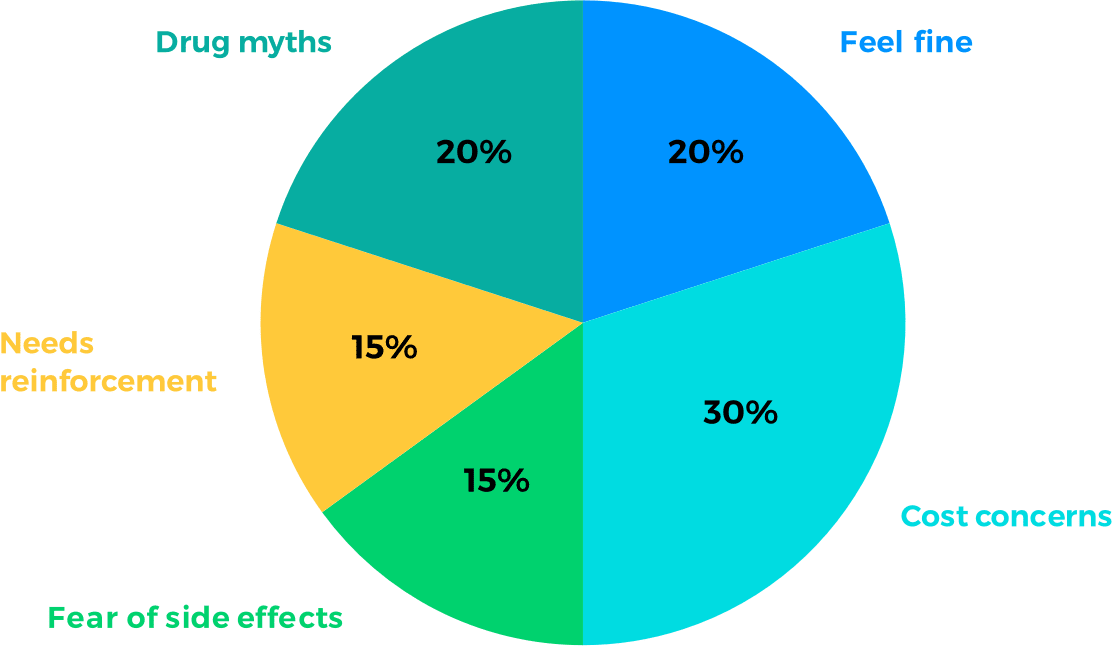
Identify and Address Member-Specific Barriers to Medication Adherence
Use claims and pharmacy gap data to understand why people are not adhering to medication –
Cost? Side effects? Lack of urgency? Other factors?
Leverage those member-specific insights to lift barriers and inspire action through personally relevant communication across pharmacy Star Rating measures.
Persuading All Members From Day One
Cater to 100% of members, based on individual decision factors, even those with little or no data through HBM’s proprietary lookalike technology.
Support chronically non-adherent members at the same priority level as adherent ones, without bias. HBM AI’s algorithm operates regardless of members’ probability to adhere, in order to better support large scale behavioral change in part D measures.
HBM Pharmacy Solution Results
Pharmacy teams equipped with the right insights on barriers to member action,
achieve higher engagement more efficiently.
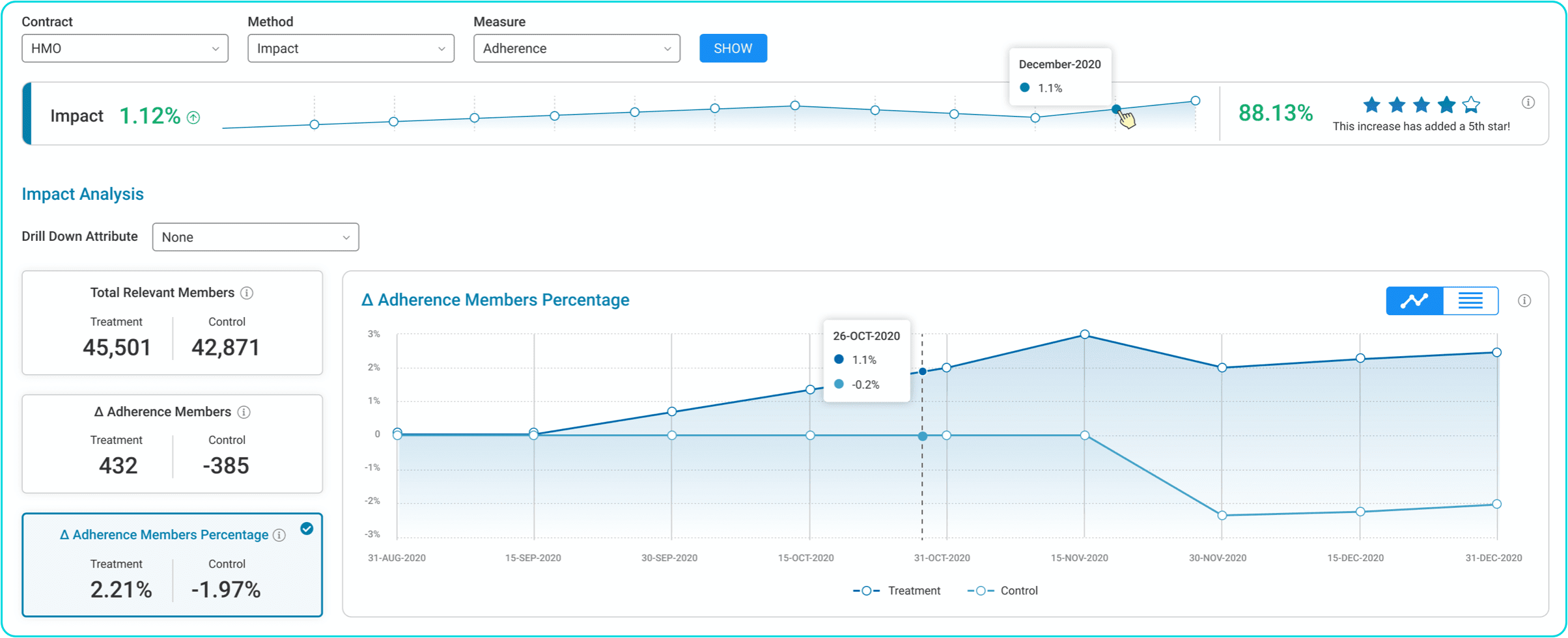
% Difference of Statin Adherent Members vs. Control
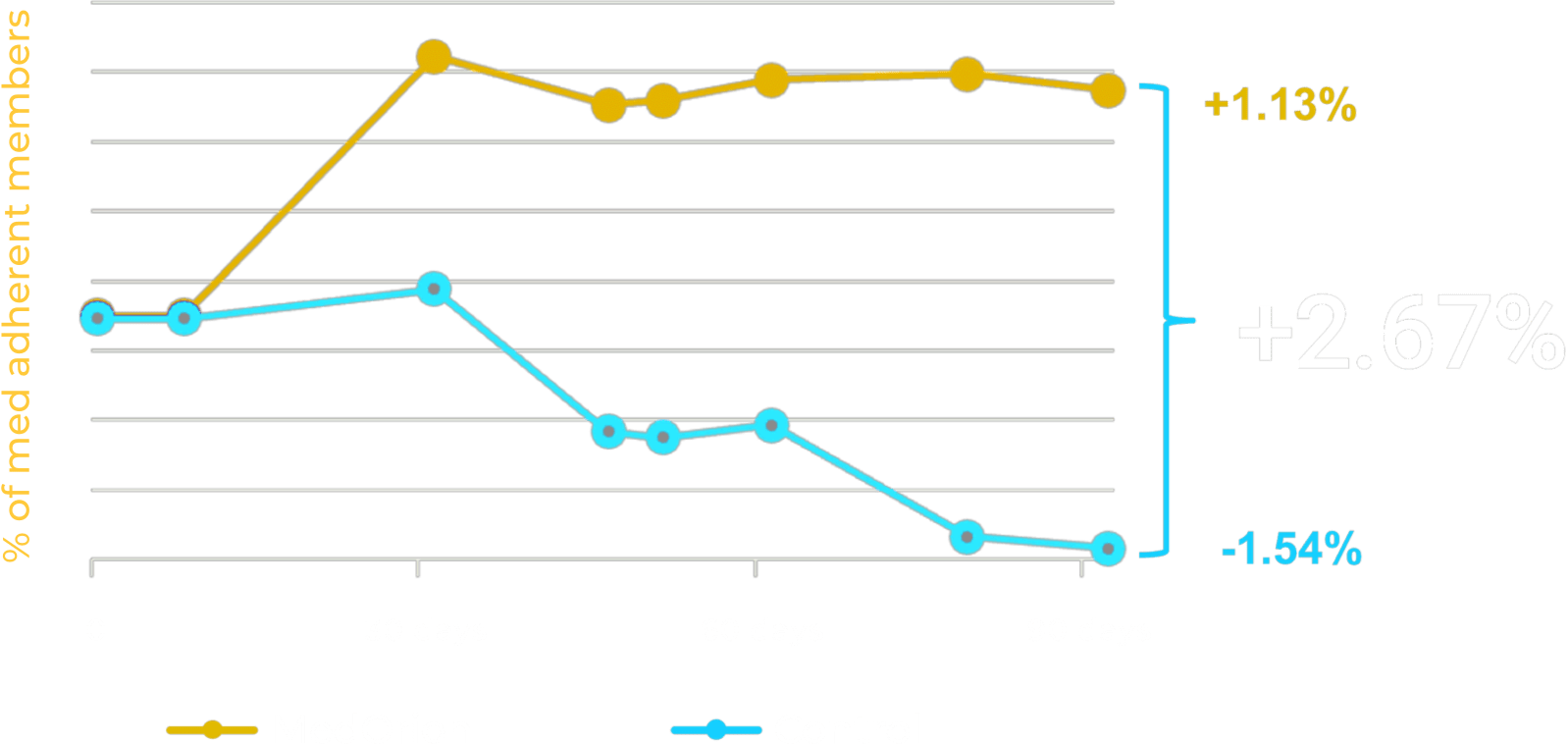
Measure Impact at the Member Level
The HBM platform self-service software lets health plans manage results through “test vs. control” groups, granting them real time visibility of individuals’ behavioral change performance.
Member level impact is continuously measured using a dedicated uplift model, then utilized for constant iterative improvement of the member journey, as well as of year-over-year outcomes.